Metastatic prostate cancer is a form of prostate cancer that has spread beyond the prostate gland to other parts of the body such as the bones, lymph nodes, or other organs. It is a serious condition that often requires aggressive treatment to slow the disease’s progression and improve quality of life. This blog post will discuss metastatic prostate cancer categories, the different treatment choices available (including recent guidelines the American Society of Clinical Oncology has published), radiation’s role in managing this condition, and where to seek care for metastatic prostate cancer in the San Francisco Bay Area.
What Is Metastatic Prostate Cancer?
Metastatic prostate cancer occurs when cancer cells from the prostate gland spread to other parts of the body through the bloodstream or lymphatic system. This condition is very serious because the cancer cells can form new tumors in other parts of the body, which can cause pain, affect organ function, and even be life-threatening. Prostate cancer cells have a proclivity to spread to the bones, and severe bone pain can sometimes be the initial symptom for men newly diagnosed with metastatic prostate cancer. It is important to note that metastatic prostate cancer is different from localized prostate cancer, which is confined to the prostate gland and can often be treated with definitive (curative) therapy in the form of surgery or radiation (including brachytherapy).
Categories of Metastatic Prostate Cancer
Metastatic prostate cancer has two main categories: hormone-sensitive and castration-resistant. Hormone-sensitive prostate cancer is still responsive to hormone therapy, which is the treatment mainstay for advanced prostate cancer. Castration-resistant prostate cancer, on the other hand, has become resistant to hormone therapy and can be more difficult to treat.
Treatment Choices for Metastatic Prostate Cancer
The treatment choices for metastatic prostate cancer depend on whether the cancer is hormone-sensitive or castration-resistant. For hormone-sensitive prostate cancer, the first-line treatment is androgen deprivation therapy (ADT), which lowers testosterone levels in the body because this hormone fuels prostate cancer growth. Lupron is a common form of ADT. The recently-published American Society of Clinical Oncology (ASCO) guidelines, adopted in early 2023, make recommendations on the first-line treatment of metastatic prostate cancer based on current data. This helpful figure by Virgo, Rumble, and Talcott from the Journal of Clinical Oncology summarizes the recommendations:
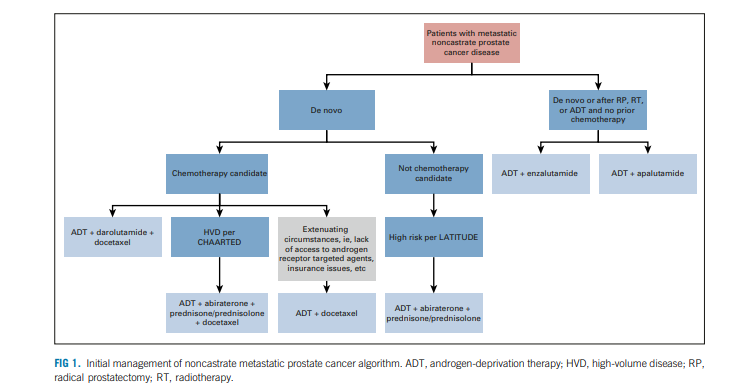
Treatment for Patients with De Novo Metastatic Prostate Cancer Who Are Candidates for Chemotherapy
For patients with high-volume metastatic prostate cancer (often defined as four or more bone metastases, one of which is outside of the spine/pelvis and/or the presence of visceral disease), a combination of androgen deprivation therapy (such as Lupron), abiraterone with prednisone, and docetaxel chemotherapy can be an excellent choice for treatment. This recommendation is based on several randomized trials, including the CHAARTED trial published in the New England Journal of Medicine. The PEACE-1 trial conclusively showed that adding abiraterone plus prednisone (to the standard of ADT and docetaxel chemotherapy) improved overall survival as compared to ADT plus docetaxel chemotherapy alone. This study was published in the journal The Lancet.
Another recent trial, the ARASENS trial, published here, included patients with metastatic prostate cancer who all received androgen deprivation therapy plus docetaxel chemotherapy. Patients were randomized to receive placebo or darolutamide (an androgen-receptor pathway inhibitor).
The study showed that adding darolutamide decreased the risk of death by 32.5% over the duration of the study for participating patients. This study paved the recommendation for ADT, plus darolutamide, plus docetaxel, as outlined in the image above.
Finally, for patients who cannot receive androgen receptor targeted agents (such as darolutamide or abiraterone), the guidelines recommend ADT plus docetaxel chemotherapy alone.
Do All Patients with Metastatic Prostate Cancer Need Chemotherapy?
Docetaxel is most recommended for patients who are diagnosed with de novo metastatic prostate cancer or patients with high-volume disease. For some patients, such as those whose prostate cancer has recurred after initial treatment with surgery or radiation therapy, ADT plus enzulutamide OR ADT plus apalutamide are very reasonable options. These patients may not need to add docetaxel chemotherapy to their prostate cancer treatment regimen.
Some patients who might otherwise benefit from chemotherapy to manage their prostate cancer cannot tolerate it due to medical contraindications or for other reasons. For these patients, ADT plus abiraterone with prednisone is a reasonable treatment option.
Other treatment options, which I won’t discuss extensively in this post, are Radium-223 (Xofigo) and Lutetium (177Lu) vipivotide tetraxetan (Pluvicto). Both are excellent treatment options for certain patients without the side effects associated with chemotherapy or androgen deprivation therapy.
What Is Radiation Therapy’s Role for Patients with Metastatic Prostate Cancer?
Radiation therapy is an essential treatment component for patients with metastatic prostate cancer. The STOPCAP systematic review and meta-analysis, published here in the journal European Urology, summarizes some of the data regarding radiation therapy’s role. This study used data from three large, randomized trials (Stampede, HORRAD, and PEACE-1) to identify the potential benefit, in terms of overall survival, for patients treated with radiation therapy to the prostate. The study found that for patients with low-volume metastatic prostate cancer (defined as fewer than five bone metastases), the addition of radiation therapy improved patients’ three-year survival rate by 7%. This improvement is significant and is on par with the improvements seen with many of the systemic therapy agents used to treat metastatic prostate cancer. Based on these data, nearly all patients with this forms of prostate cancer should at least meet with a radiation oncologist to discuss whether radiation therapy’s potential benefits outweigh any of its potential harms.
Can Patients with Metastatic Prostate Cancer Use Radiation Therapy to Delay or Avoid Androgen Deprivation Therapy?
ADT is the mainstay treatment for patients with metastatic prostate cancer. However, ADT also comes with many side effects, such as fatigue, loss of libido, hot flashes, and weight gain. One of my favorite clinical trials in this space is the STOMP trial, which was a multi-center, phase 2, randomized trial that enrolled asymptomatic prostate cancer patients who were eligible for treatment after biochemical recurrence following primary radiation or surgery treatment. All patients had hormone-sensitive prostate cancer with up to three bone metastases. Patients were randomized to surveillance-alone versus metastases-directed therapy, typically with high-dose SBRT radiation therapy to all disease sites. The study found that the ADT-free survival rate (the percent of patients who were alive and did not receive subsequent ADT treatment) was 8% for the surveillance group versus 34% for the metastases-directed therapy group.
The ORIOLE trial, published in JAMA Oncology randomized 54 patients with hormone-sensitive prostate cancer and between one and three metastases who had not received ADT within six months of trial enrollment to either observation or treatment with SBRT radiation to all disease sites. Treatment with SBRT improved median progression-free survival and induced a systemic immune response. These data again showed the importance of integrating radiation therapy into the treatment of oligometastatic prostate cancer.
Finally, the EXTEND study, a randomized clinical trial published by Dr. Chad Tang and colleagues in JAMA Oncology in 2023 randomized patients with metastatic prostate cancer to intermittent ADT versus intermittent ADT with metastases-directed therapy (typically with SBRT). A total of 87 patients were included in the study. The primary endpoint in the study was disease progression and a secondary endpoint was eugonadal PFS (or time from testosterone recovery after ADT to disease progression). Both outcomes were significantly improved with metastases-directed therapy.
In summary, all these trials show that the use of radiation therapy in well-selected patients can both improve their overall survival rate and their quality of life by potentially delaying or reducing the use of androgen deprivation therapy.
Getting your Treatment at El Camino Hospital in the San Francisco Bay Area
El Camino Hospital, located in Mountain View, CA, is a leading cancer center for patients diagnosed with prostate cancer. El Camino Hospital has a comprehensive cancer center that has access to the latest treatments, including the Ethos adaptive radiation therapy system and radiopharmaceuticals, as well as well regarded physicians across medical oncology, urology, and radiation oncology. Physicians at El Camino Hospital treat patients with prostate cancer from throughout California and Arizona. I encourage patients diagnosed with metastatic prostate cancer to seek second opinions with my medical oncology colleagues, Dr. Shane Dormady, Dr. Jiali Li, and Dr. Shiva Singhal here: https://www.elcaminohealth.org/doctors
Conclusion
The treatment of metastatic prostate cancer is rapidly changing, with advances in options for hormone manipulation, chemotherapy, radiopharmaceuticals, and metastases-directed therapy with radiation therapy. These advances not only allow patients to live longer lives, but they also improve patients’ quality of life.
About the Author
Dr. Ankit Agarwal is a radiation oncologist/brachytherapist who specializes in the treatment of prostate cancer and lives in the San Francisco Bay Area. Dr. Agarwal has published extensively on the treatment of prostate cancer and has treated patients with prostate brachytherapy in North Carolina, California, and Arizona. If you are in California or Arizona and would like to consult with one of Western Radiation Oncology’s physicians, please contact us here. Details on our Southern California clinic can be found here, and details on our Arizona clinic location can be found here.
